Paracetamol (acetaminophen) is among the most widely used analgesics worldwide. But does it live up to its reputation as a safe and effective painkiller? This 2021 overview consolidates findings from 10 Cochrane systematic reviews, covering over 20,000 participants, to reassess the efficacy and safety of paracetamol across a range of acute and chronic pain conditions.
🔍 Key Findings
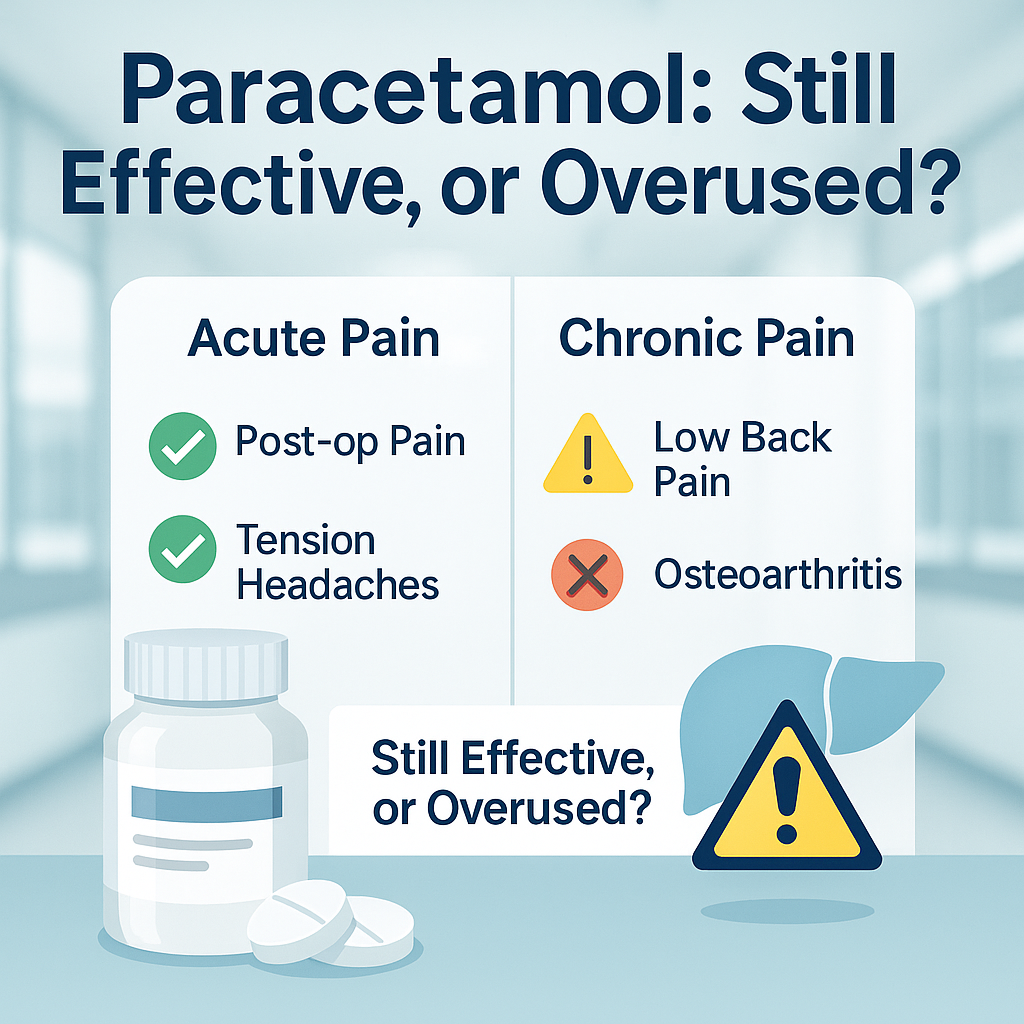
✅ Where It Works
- Acute pain (e.g., postoperative pain, tension headaches):
Moderate evidence supports paracetamol’s efficacy.- In post-surgical pain: ~50% achieved ≥50% pain relief with a single 1,000 mg dose.
- In tension-type headaches: Slight benefit over placebo, but less than NSAIDs.
❌ Where It Doesn’t Work Well
- Chronic pain conditions:
- Low back pain: No significant benefit over placebo.
- Hip/knee osteoarthritis: Only very modest pain relief, not clinically meaningful.
- Cancer pain: Limited data; paracetamol is often used as adjunctive, not primary therapy.
⚠️ Safety Concerns
- Generally safe at therapeutic doses, with a strong safety record over decades.
- However, risk of liver toxicity increases sharply with overdose or long-term misuse.
- Widespread OTC availability may lead to public overconfidence in its safety profile.
- Concerns also noted around combination products with opioids, which may obscure toxicity risk.
🧠 Clinical Implications
- For acute, self-limiting pain, paracetamol remains a reasonable first-line choice.
- For chronic musculoskeletal conditions, clinicians should reconsider its use—particularly as a standalone therapy.
- Emphasizes the importance of shared decision-making, especially for long-term users with limited benefit.
📣 Promotional Angle
“Is it time to rethink the world’s favorite painkiller?”
This review is ideal for patient education campaigns, pharmacy training modules, or medical blogs targeting both consumers and practitioners. It invites readers to critically evaluate a common household drug and encourages smarter, safer pain management strategies.