An In-Depth Website Summary of Xia & Heeringa’s “Psychopathology and the Human Connectome”
🔍 Introduction
The 21st-century revolution in neuroscience has radically reshaped our understanding of mental illness. No longer seen solely as chemical imbalances or isolated dysfunctions in specific brain regions, psychiatric disorders are now increasingly conceptualized as network-level disorders of the brain—the result of disturbed connectivity within and between large-scale neural systems.
At the forefront of this paradigm shift is the connectome: a comprehensive map of neural connections within the brain. This groundbreaking paper by Xia and Heeringa systematically explores how the human connectome can help us understand, diagnose, and potentially treat a wide range of psychopathologies.
🧬 What Is the Human Connectome?
The human connectome refers to the complete mapping of neural connections in the brain, comprising two major types:
- Structural Connectivity – the physical “wiring” of the brain via axonal pathways
- Functional Connectivity – statistical correlations between activity in different brain regions, often measured by resting-state fMRI
Modern imaging technologies (e.g., diffusion tensor imaging, fMRI, graph theory) allow researchers to represent the brain as a complex network of nodes (brain regions) and edges (connections).
Understanding mental illness through this lens involves identifying patterns of disrupted connectivity that correlate with clinical symptoms, behavioral deficits, or cognitive impairments.
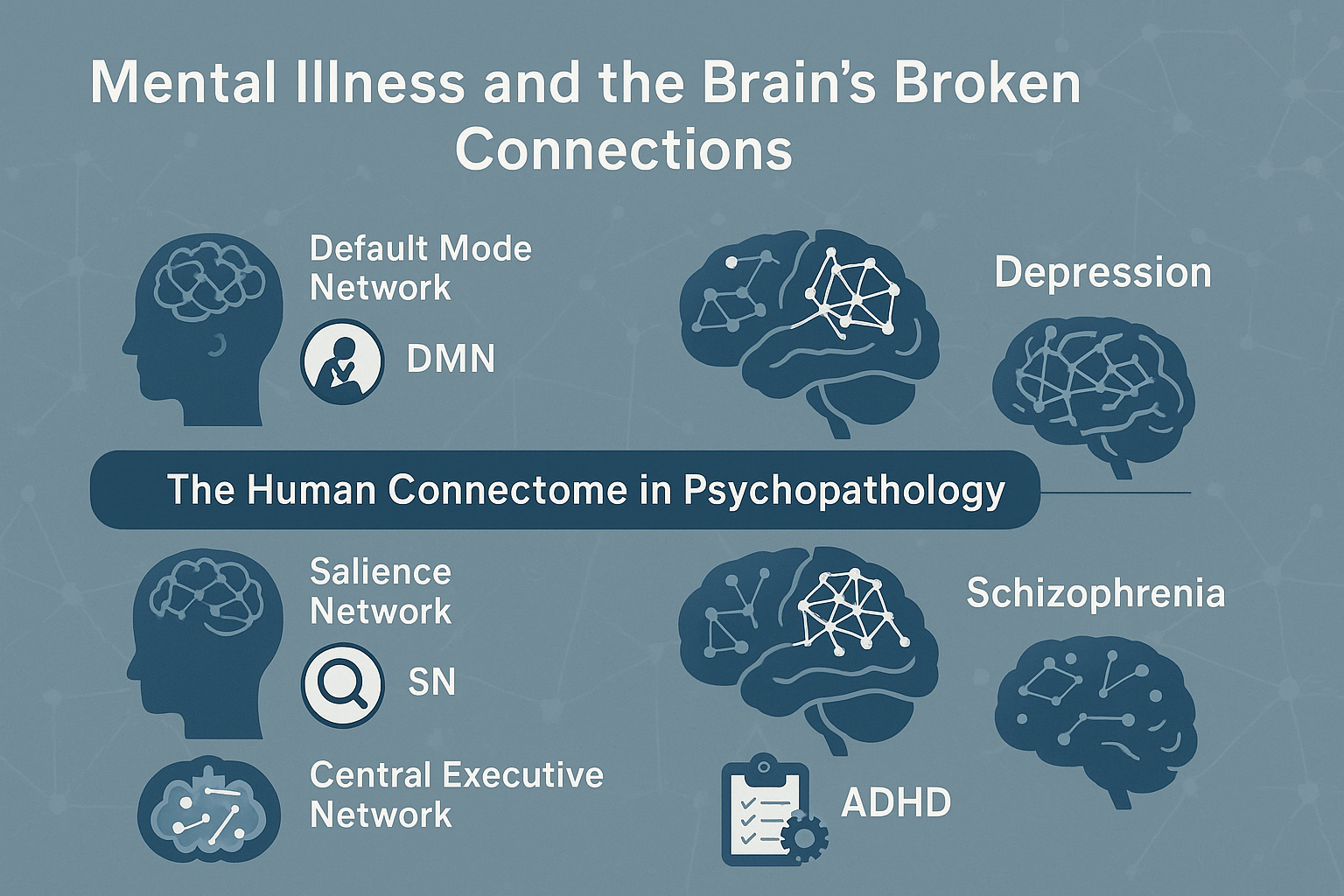
🧠 Core Brain Networks in Mental Health
Xia and Heeringa focus on three key intrinsic connectivity networks (ICNs) that are central to understanding psychopathology:
1. Default Mode Network (DMN)
- Active during rest and internal thought (e.g., daydreaming, self-referential processing)
- Dysfunctions linked to:
- Depression (excessive rumination)
- Schizophrenia (aberrant self-processing)
- ADHD (failure to suppress DMN during task)
2. Salience Network (SN)
- Detects and filters relevant internal and external stimuli
- Anchored in the anterior insula and anterior cingulate cortex
- Dysfunctions found in:
- Anxiety disorders (overactive threat detection)
- Schizophrenia (hallucinations, delusions)
- Autism spectrum disorders
3. Central Executive Network (CEN)
- Supports goal-directed behavior and cognitive control
- Includes dorsolateral prefrontal cortex and posterior parietal cortex
- Impaired in:
- ADHD
- PTSD
- Bipolar disorder
These three networks interact dynamically. Effective mental functioning depends on the ability to switch between them flexibly. Dysfunction in this dynamic switching process is a hallmark of several psychiatric conditions.
📊 Transdiagnostic Themes in Connectome Research
Rather than treating each disorder as isolated, connectome studies have revealed transdiagnostic patterns—common neural signatures across multiple psychiatric illnesses.
For example:
- DMN hyperconnectivity → depression, schizophrenia, and OCD
- Salience network dysregulation → both PTSD and psychosis
- Executive control impairments → seen in ADHD, addiction, and MDD
This supports initiatives like RDoC (Research Domain Criteria) that aim to replace rigid DSM categories with neural circuit-based models.
🧪 Measuring Connectivity: Methods and Metrics
The article introduces key concepts and techniques used in connectomics:
- Resting-state fMRI (rs-fMRI): measures temporal correlations of activity across brain regions
- Diffusion MRI: maps white matter tracts (axons)
- Graph Theory Metrics:
- Node Degree: number of connections a region has
- Modularity: degree of segregation into subnetworks
- Global Efficiency: capacity for information transfer across the brain
- Machine Learning: increasingly used to classify disorders based on connectivity “fingerprints”
These tools help researchers identify biomarkers and endophenotypes that bridge the gap between genes, brain structure, and behavior.
🧬 Development, Genes, and Environment
Connectome architecture is developmentally sensitive and genetically influenced:
- Adolescents show increasing connectivity in executive networks, explaining impulsivity and risk-taking
- Early trauma may permanently disrupt SN and CEN, increasing vulnerability to PTSD and mood disorders
- Genetic studies show high heritability of functional connectivity patterns, especially in frontoparietal circuits
Environmental exposures (e.g., poverty, chronic stress) can also lead to altered connectome configurations—suggesting a pathway from social adversity to neural dysfunction.
🧠 Connectomics in Specific Disorders
1. Schizophrenia
- Reduced global efficiency and impaired network integration
- Dysfunctional thalamocortical connectivity
- Fragmented default mode and salience networks
2. Depression
- Hyperactive DMN (linked to rumination)
- Weak CEN activity (impaired cognitive control)
- Abnormal amygdala-prefrontal coupling
3. ADHD
- Delayed maturation of frontostriatal circuits
- Poor anti-correlation between DMN and task-positive networks
- Disrupted reward processing circuits
4. PTSD
- Impaired top-down regulation from prefrontal cortex
- Enhanced amygdala connectivity
- Fragmented hippocampal integration
Each disorder involves unique yet overlapping patterns of network dysfunction, reinforcing the idea of dimensional, circuit-based psychopathology.
💡 Clinical Applications and Future Prospects
Diagnostic Tools
- Connectome-based classifiers may enable early identification and subtyping of mental illness
- Example: Functional connectivity can predict risk for psychosis in youth at high clinical risk
Personalized Treatment
- Brain-based profiles could inform treatment selection (e.g., who will respond to CBT vs. SSRIs)
- Neurofeedback and TMS protocols may be tailored to specific network abnormalities
Prognosis and Monitoring
- Longitudinal studies suggest that connectivity changes over time can track treatment response and disease progression
🧭 Ethical and Methodological Challenges
While promising, connectome-based psychiatry faces challenges:
- Individual variability in brain networks complicates group-level generalizations
- Risk of neuro-essentialism (reducing identity to brain networks)
- Need for replication, diverse populations, and standardized pipelines
Nevertheless, the field is progressing toward a precision psychiatry model, where brain connectivity is central to understanding and treating mental illness.
📣 Conclusion
“Mental disorders are not errors of brain parts, but of brain conversations.”
This comprehensive review by Xia & Heeringa makes it clear: to understand the mind, we must map the dynamic architecture of the brain. The connectome approach offers a unified framework to bridge clinical symptoms with underlying biology, transcending outdated diagnostic silos.
As technologies evolve and datasets grow, connectome-informed psychiatry holds the potential to transform both diagnosis and care, making mental health treatment more biologically grounded, individualized, and effective.